Updated: July 24th, 2023
Sexually transmitted infections (STIs), sometimes referred to as sexually transmitted diseases (STDs), are infections that are primarily passed from person to person during sexual contact. The most common STIs identified worldwide are gonorrhea, chlamydia, syphilis, herpes, human papillomavirus (HPV), HIV/AIDS, and trichomoniasis, as well as emerging STIs like Ureaplasma and Mycoplasma. Grasping their symptoms, knowing the right time to test and retest for these infections, understanding treatment options, and acknowledging the importance of retesting—even after successful treatment—can greatly impact your sexual health management.
Symptoms of Most Common STIs
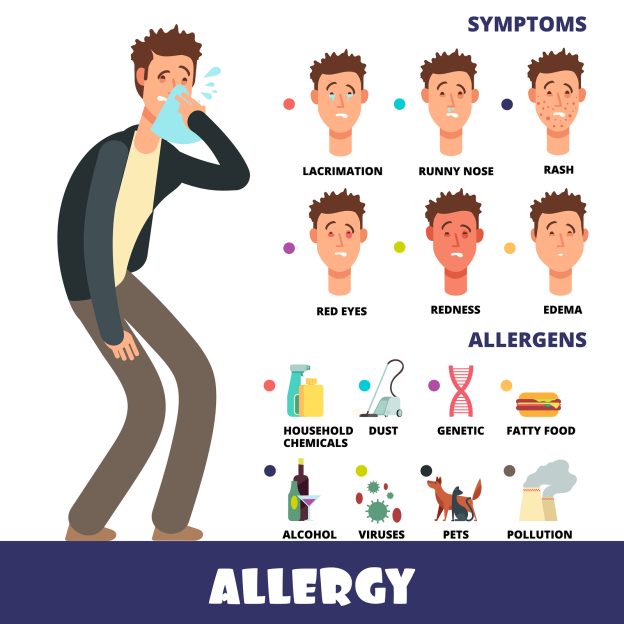
Although some STIs can show no symptoms, below are common symptoms associated with each infection:
- Gonorrhea and Chlamydia: Symptoms may include unusual discharge, a burning sensation during urination, and in men, pain or swelling in one or both testicles. Women may experience pain during intercourse, lower abdominal pain, or a low-grade fever.
- Syphilis: This infection often begins as a painless sore on the genitals, rectum, or mouth. As it progresses, it can lead to rashes, fever, swollen lymph nodes, and fatigue.
- Herpes: Herpes is characterized by outbreaks of blisters and sores around the mouth or genital area. The virus stays dormant in the body between outbreaks.
- HPV: Some types of HPV can lead to genital warts, while others may not cause symptoms but can lead to various cancers.
- HIV/AIDS: Early symptoms of HIV/AIDS include flu-like symptoms. As it progresses, it can lead to weight loss, fever, night sweats, and fatigue.
- Trichomoniasis: This STI can cause itching or irritation inside the penis, burning after urination or ejaculation, and some discharge from the penis in men. Women might notice itching, burning, redness or soreness of the genitals, discomfort with urination, or a thin discharge with an unusual smell that can be clear, white, yellowish, or greenish.
- Ureaplasma and Mycoplasma: Many individuals with these infections don’t experience symptoms. However, when present, symptoms can include burning or pain during urination, urethritis, or more complex reproductive and urinary tract disorders.
Testing and Retesting for STIs
Determining the right time to test for an STI post-exposure depends on the specific infection. General guidelines are:
- Gonorrhea and Chlamydia: Test 5 days weeks after exposure or for any symptoms.
- Syphilis: Test 1-3 weeks for primary syphilis.
- Herpes: Test 2 weeks to 3 months after exposure.
- HPV: No approved test for men; women should have regular screenings as part of Pap tests.
- HIV: Test 1-3 months after exposure.
- Trichomoniasis: Most people are diagnosed when a partner reports symptoms; testing can occur as soon as symptoms are reported.
- Ureaplasma and Mycoplasma: Testing should be considered if you have symptoms or risk factors like multiple sexual partners or unprotected sex.
Retesting after treatment is crucial to ensure the infection has been completely eradicated and to check for potential reinfections.
Treatment Options
Treatment plans differ based on the STI:
- Gonorrhea, Chlamydia, Syphilis, and Trichomoniasis: These bacterial infections are typically treated with antibiotics.
- Herpes and HIV: These viral infections can’t be cured, but their symptoms can be managed with antiviral medications.
- HPV: Treatment often focuses on managing symptoms and regular monitoring for potential cancer development.
- Ureaplasma and Mycoplasma: These infections are generally treated with antibiotics; however, antibiotic resistance can be an issue, particularly with Mycoplasma genitalium.
Understanding the intricacies of STIs, from their symptoms to their treatment options, is essential for managing your sexual health. Always remember the mantra: “Get tested, get treated, and get retested”. Knowing your status empowers you to maintain a healthy lifestyle and make informed choices.
To support your sexual health management, consider getting tested today at our partner labs, which provide low-cost, fast turnaround time, and easy scheduling for your convenience. Knowing your status not only empowers you to make informed choices but also contributes to overall health.